At least two in five U.S. adults — or more than 57 million people – under the age of 65 with “private insurance could be eligible under clinical criteria for GLP-1 drugs,” a new analysis shows.
KFF, formerly known as the Kaiser Family Foundation, that 42% of U.S. adults could pass muster of health insurers if they are treated with “type 2 diabetes, obesity, or excess weight and weight-related health issues, according to a new KFF analysis.
“Though only about 3% of adults with employer coverage had a prescription in 2022, demand for and spending on GLP-1 drugs has grown and could continue to grow,” KFF said in its analysis. “Given the steep costs and high demand for these drugs, employers and insurers may continue to impose more restrictive eligibility standards for coverage than the clinical indications set by the Food and Drug Administration. Many private plans manage the costs associated with GLP-1 drugs by only covering them for diabetes treatment and not for weight management.”
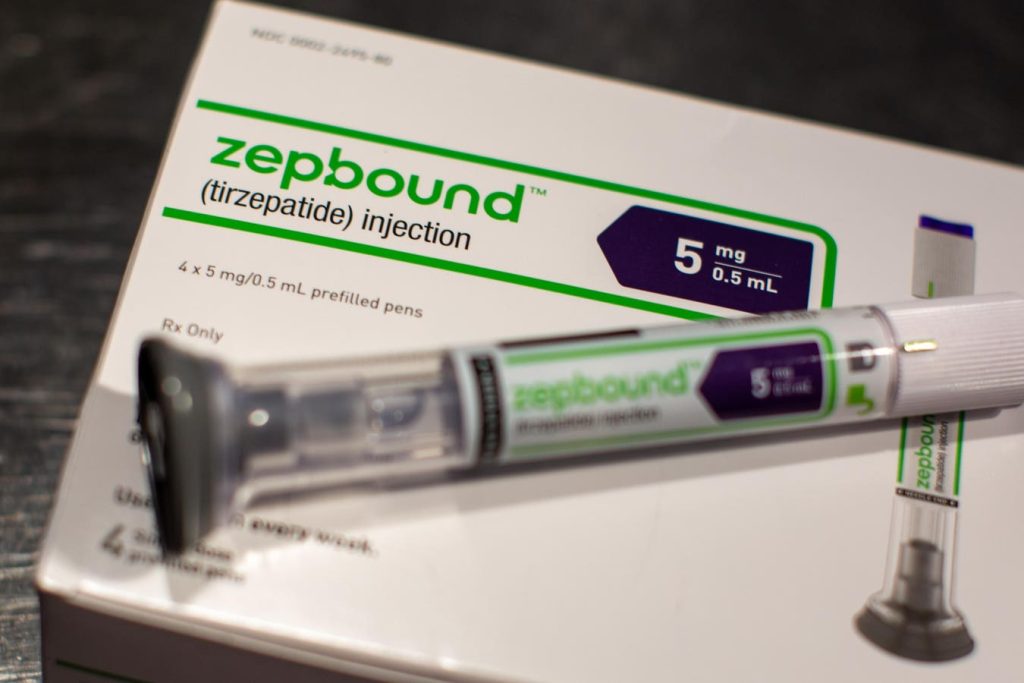
Still, these drugs, which include Wegovy, Rybelsus and Saxenda—along with Ozempic and Zepbound—will be the “single biggest driver” of employer health costs, adding 1% to the total premium expense for 2025, new data from the benefits consultancy Aon says.
KFF’s analysis tells a similar story that policymakers, employers and patients should be bracing for, writers of the report indicate.
Citing annual filings with state regulators for the 2025 health coverage year, KFF said “some insurers cited increases in utilization of GLP-1 drugs as a contributor to rising premiums.”
Most employees and others with private health insurance coverage will first see what they will pay in premiums and co-payments this fall when they take a look at their 2025 benefits during open enrollment, the annual ritual when workers can choose or change their health benefit choices. They will also notice the kinds of restrictions health plans will place on whether they can even get their GLP-1 drugs paid for, analysts say.
“Many ACA Marketplace plans manage the costs associated with GLP-1 drugs by only covering them for diabetes treatment and not for weight management,” KFF said.
“These broad estimates indicate the potential number of non-elderly adults who meet the clinical criteria for GLP-1 drugs, although employers and insurers may have more restrictive eligibility standards for coverage,” KFF’s analysis said. “Additionally, because many people with diabetes or who are overweight may control their condition with diet, other medications and therapies, or choose to not seek treatment, not all people who meet these clinical criteria would use GLP-1 drugs.”
Read the full article here