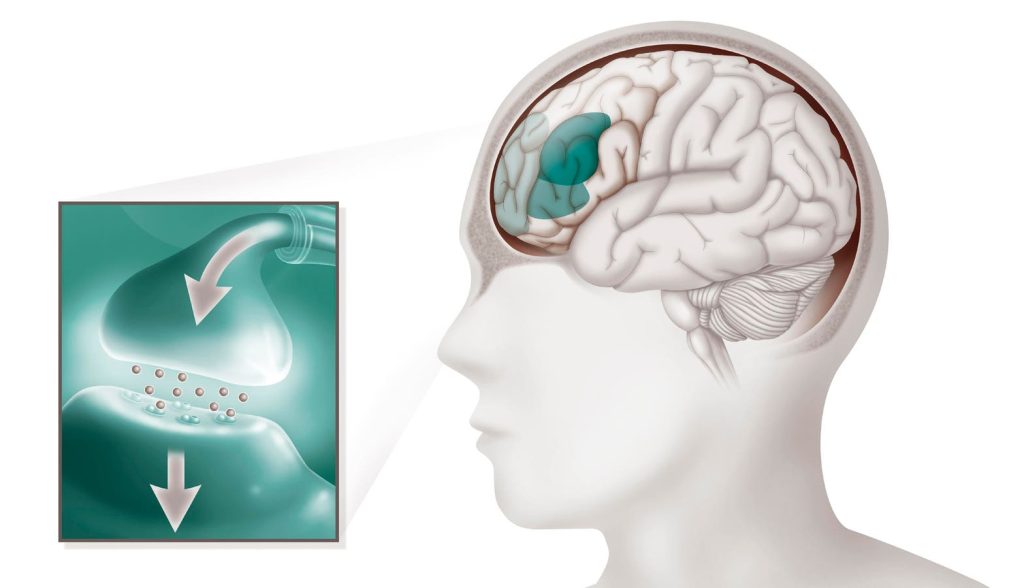
A new study that included 221,714 adults and adolescents with attention-deficit/hyperactivity disorder (ADHD) found that those who were prescribed ADHD stimulant medications were at a lower risk of attempting suicide or dying by suicide. Additionally, the use of ADHD medications was also associated with fewer psychiatric hospitalizations.
Heidi Taipale, a researcher at Karolinska Institute in Stockholm, Sweden, and colleagues, observed that four ADHD medications were linked to a decreased risk of being hospitalized due to psychiatric co-morbidities — amphetamine, lisdexamphetamine, dexamphetamine, and methylphenidate.
Whereas a decreased risk of suicidal behavior was only associated with using lisdexamphetamine, dexamphetamine, and methylphenidate. A 2019 study conducted in Sweden revealed that the prevalence of psychiatric co-morbidity was 52% among children and adults with ADHD. In comparison, the prevalence is only 7% among individuals without ADHD. A psychiatric co-morbidity includes conditions like major depressive disorder, panic disorder, substance abuse, generalized anxiety disorder, agoraphobia, obsessive-compulsive disorder, PTSD, and psychotic symptoms.
The 2019 study further reported that psychiatric co-morbidity increased the risk of mortality among people with ADHD, particularly when the comorbidity was substance use disorder.
Taipale and team noted that while an ADHD medication called atomoxetine was not linked to a lower risk of psychiatric hospitalizations or suicidal behavior, they found an association between atomoxetine and fewer hospitalizations for non-psychiatric co-morbidities.
“In addition to ADHD core symptoms, there is considerable evidence that ADHD medications, especially stimulants, improve functioning and quality of life. Less is known about the long-term effectiveness and safety of ADHD pharmacotherapies,” the researchers wrote.
“Because ADHD medications in long-term observational studies are associated with both beneficial psychiatric outcomes, such as decreased risk of depression and suicide, and with possible adverse outcomes such as the risk of psychosis, we aimed to investigate the association of specific ADHD medication use with the risk of psychiatric hospitalization in a nationwide cohort of adolescents and adults with ADHD,” they added.
In this study, the team included people between the ages of 16 to 65 years old who were residing in Sweden and had received an ADHD diagnosis between 2006 to 2021. They then analyzed the study participants’ inpatient and outpatient healthcare data that they had collected from the Swedish National Patient Register.
The researchers were able to track which study participants were purchasing prescribed ADHD medications through data they had obtained from the Prescribed Drug Register. Methylphenidate was the most commonly used ADHD medication among 68.5% of the cohort, followed by lisdexamphetamine (35.2%) and atomoxetine (15.6%).
The study participants underwent a follow-up period that lasted for 15 years. Out of the 221,714 study participants, 56% had a psychiatric comorbidity. Anxiety, depression, bipolar disorder, and stress-related disorders were the most common ones. Close to 26% of them had been hospitalized due to a psychiatric co-morbidity.
Interestingly, while lisdexamphetamine was associated with a decreased risk of psychiatric hospitalizations among adolescents, young adults, and adults aged 30 and older, methylphenidate seemed to be less effective among older adults.
“It seems that methylphenidate either is less effective among those aged 30 years or older or there is some kind of initial effect that diminishes with longer-term use, age, or course of illness because methylphenidate is usually prescribed as the first-line medication,” the researchers explained. Whereas atomoxetine was linked to a decreased risk of hospitalization among women but not men.
“The overall effect on psychiatric outcomes was beneficial, and, similarly, we found a decreased (rather than increased) risk of non-psychiatric hospitalizations. There are concerns that long-term stimulant use may be associated with adverse outcomes. Because these medications tend to increase blood pressure and heart rate, they might increase the risk of cardiovascular diseases. An increased risk of seizures, and possibly an increased risk of psychosis or mania, are also concerns,” the researchers highlighted.”
The study was published online on JAMA Network Open on March 20, 2024.
Read the full article here